Released today, an independent report of the service's nine year history commissioned by the South Island Alliance Leadership Team pulls no punches.
It paints a picture of a service which has struggled to provide adequate neurosurgery services in Dunedin for the past nine years, and which has major ongoing issues attracting staff to live and work in the city.
At no time had stable staffing in Dunedin with three neurosurgeons been achieved.
"The past history is a litany of unfulfilled expectations and early departures,'' the report said.
"The team is not confident that the staffing structure is any more durable than at any time in the previous three triennia.''
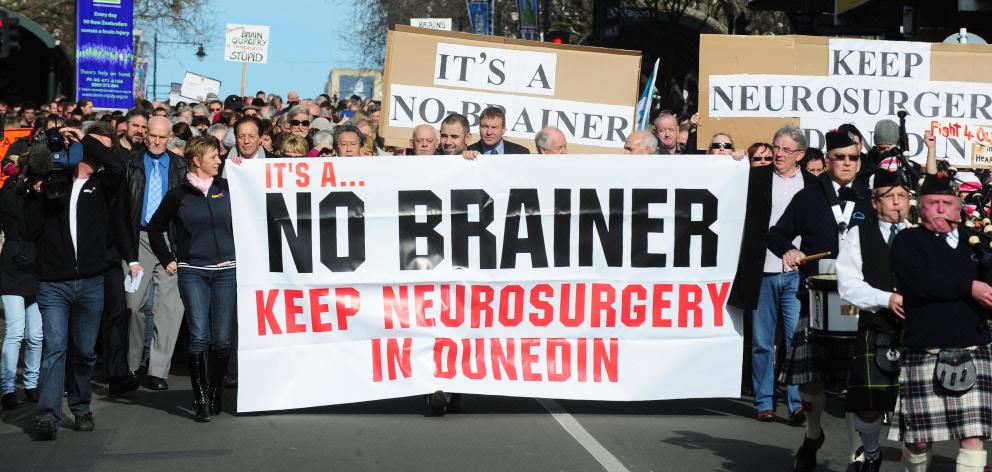
A massive public campaign, spearheaded by the Otago Daily Times, in 2010 led to neurosurgery services, under threat of centralisation in Christchurch, being maintained in Dunedin.
A subsequent fundraising campaign resulted in $3 million raised to fund a chair in neurosurgery at the University of Otago.
The report panel was chaired by Auckland surgeon Ian Civil and comprised Scottish neurosurgeon Jennifer Brown, Auckland nurse unit manager Denise Le Lievre and South Island Alliance programme manager Janice Donaldson.
The panel first considered whether recommendations of the 2010 expert panel report, which established the South Island Neurosurgery Service (SINS), had been adopted, before assessing the current state of the service.
"The service has never functioned, or been funded, managed, or staffed on a 'one service, two sites' basis,'' the report said.
"Supportive links between clinical staff in surgery, nursing and allied health and technical services are rudimentary at best . . . rather than a single service delivered on two sites, as recommended by the expert panel report, we saw two small units with competing interests and witnessed evidence of a relationship marked by mistrust.''
The original governance board for the service only existed until December 2012.
The report said the current model did not meet the objectives of the original plan, and saw board members appointed indefinitely and seemingly without terms of reference.
Plans for a publicly available six monthly report had long since fallen by the wayside.
"There were a range of other documents containing data evident in the papers of the SINS board subsequent to March 2013, but nothing resembling an overall board report containing activities, data, achievements and plans either six monthly, or annually.''
The report made 13 recommendations, which included:
- Setting up a national clinical network for neurosurgery;
- Reconstituting the SINS board and making it independent of South Island health boards'
- Restricting on-call hours to assist patient and clinician safety;
- Reassess funding models.
SINS chairman Chris Fleming said the service accepted 12 of the report's recommendations, but rejected its suggestion that recruitment of clinical staff be uncoupled from recruitment of University of Otago staff.
"We are fortunate in the South Island that we all share the same goal,'' Mr Fleming, who is also the Southern District Health Board chief executive, said.
"We look forward to implementing these recommendations to further improve the quality and sustainability of the South Island Neurosurgery Service.''
Mr Fleming said the report set out some of the difficulties the Alliance had faced maintaining neurological services, and made recommendations for the future.
"We remain committed to a South Island-wide service that includes a Dunedin presence for a neurosurgical speciality services,'' he said.
"We look forward to working with our colleagues in the South Island Neurosurgical Service to take further steps to build a strong service that recognises the practical constraints we are facing.
"We also remain committed to our partnership with University of Otago, and continuing to exploring the opportunities that come from the joint clinical and academic positions as part of a sustainable service.''
Dunedin still has just one full-time neurosurgeon; Mr Fleming said recruitment efforts were continuing for permanent and/or locum staff.
Comments
These appear to be managerial/administrative concerns. No patients have died under neurosurgery at DPH; one has, at Christchurch.
I am sorry Hill, apro your comment regarding deaths in the different units, unless you work in the system and are involved with the morbidity and mortality audit that takes place on a quarterly and annual basis, you should refrain from comments like this. Please get a copy of the full report by the review committee and next time you have a neurosurgical condition or emergency, make an unbiased call as to where you should be getting your treatment. I think you will be left in no doubt!












