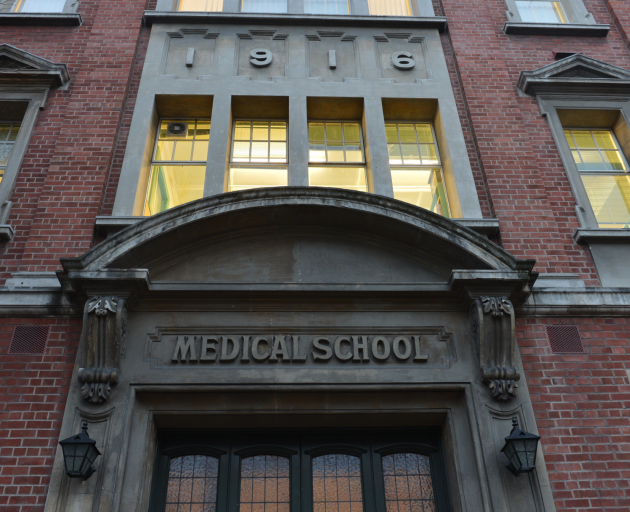
Collaboration between Dunedin Hospital and the Otago Medical School must continue, Emeritus Prof Gil Barbezat writes.
Dunedin Hospital has a long and proud record of providing for the health needs of our community. This relates not only in caring for the sick, but also in educating many generations of a variety of health professionals. Its association with the Otago Medical School has spawned many distinguished health professionals now widely distributed all over the world. Indeed, this association has resulted in many professionals being recruited to the University of Otago who would not otherwise have come to our province.
This hospital is currently in the news headlines relating to its rebuild. Rumours abound about what this will entail. Reading the ODT, the word ``downgrading'' appears far too often for comfort, especially when it is linked to the controversial Sapere Report. It has been very difficult to pry out any official comments about this situation. The fact hospital governance has been devolved to government appointees, without the region's democratic election of board members, does nothing for confidence in the process.
The quality of data for decision-making is crucial. If the Sapere Report is an example, we do need to be concerned. Staff employed primarily by the hospital and medical school were alarmed by the tenor and content of that report. Heads of clinical departments had no idea who had been consulted; nobody identified as contributing to the information.
Accusations of seeing patients unnecessarily for purely academic purposes were met with disbelief. Clinicians are overloaded and would welcome reductions in patient numbers through increased follow-up in the community. Overprescribing expensive medications by academic staff is preposterous, as such prescriptions are closely controlled by Pharmac. Indeed, many academics are involved in developing national guidelines for patient management. In my early retirement, I was employed by Pharmac to educate medical practitioners how to use some of these medications appropriately. Drug trials conducted by staff obtain medications funded by industry, saving hospital expense. Staff recruitment and retention is greatly enhanced by the collaboration between the hospital and medical school.
Concerns about the funding of a teaching hospital are not new. Over the nearly 40 years of my association with Dunedin Hospital and the medical school, we have had two extensive formal reviews of how these two institutions relate to each other.
The first was the Palmerston North Report in 1983. Des Hessian (representing the then Otago Hospital Board) and I (Medical School) painstakingly analysed the clinical throughput of both Palmerston North (non-teaching) and Otago (teaching) Hospital Boards for a given time period. Dr Karen Poutasi helped with the data analysis. We showed that staff-patient ratios, outpatient visits, pharmacy costs and inpatient day stay were all more efficient in Otago. Some tertiary specialist services (not available elsewhere) understandably incurred some extra cost.
The second was in 1997, when Suzanne Snively was commissioned (through PWC) to compare the daily activities of staff from both the hospital and medical school. Not surprisingly, she showed that both institutions were of mutual benefit to each other.
How often is it necessary to reinvent the wheel? Collaboration between both institutions must be considered in future planning to benefit the people of Otago and Southland. Patient care is crucial in this equation, but also the research-based quality of our New Zealand health professional graduates. The future demands adequate and appropriate investment in both.
Dunedin Hospital has a broad representation of specialists for very good reasons. The local public confirmed their support of this when we took to the streets to demonstrate against the threat of removing neurosurgery. Exactly how these services are used requires debate, balancing general with specialist needs. Both secondary and tertiary demands will increase, not decrease. For example, a bowel-screening programme is imminent; well trained staff and facilities are required for this. Dunedin has trained its first nurse endoscopist, and leads the country in this way. Demands on specialist surgery will increase when more bowel cancers are operated on in time to save lives. However, theatre space is still required for patients presenting with acute appendicitis.
Specialist clinical departments often link with basic science departments in our university to provide benefits for all New Zealanders. As an example, the gene mutation responsible for stomach cancer in our Maori population was discovered in our biochemistry department, after collaboration with clinical departments. Many more such collaborations could be cited.
Last but not least, I repeat a plea that this debate is conducted with valid data, not in secret, and with responsible participation of those involved. While political opinions must be considered, they cannot be allowed to dictate the final outcome. Dunedin Hospital must be recognised as a major clinical and teaching facility, and not downgraded. People of Dunedin must rally to ensure we stand by this valuable institution.
Emeritus Prof Gil Barbezat is a retired gastroenterologist and former gastroenterology and medicine department head.