Q: What were the most striking features of the 1918 influenza pandemic?
A: It had a very high death toll, around 2 per cent of the global population, or around 60 million people. In New Zealand 9000 died during two months. The illness itself was very different to this coronavirus in that it knocked people down very quickly. It prostrated you, so that you couldn't get out of bed. It came with a high fever, a lot of sweating, a shortness of breath.
One of the most terrifying things was that it was hitting young adults. And the bodies turned black, due to a process called cyanosis, because their lungs weren't getting any oxygen. That's what started me on the whole process of writing my book, I was talking to my father who was a boy in Taumarunui at the time, about going to check on people with his father. He told one story where they went to check the neighbours and the wife was sound asleep and the husband had died and gone black. Can you imagine it? People were very scared.
Q: Why was its impact so severe?
A: The world was at war, so there were lots of troops moving around the world - including coming back to New Zealand where they then scattered back to their homes.
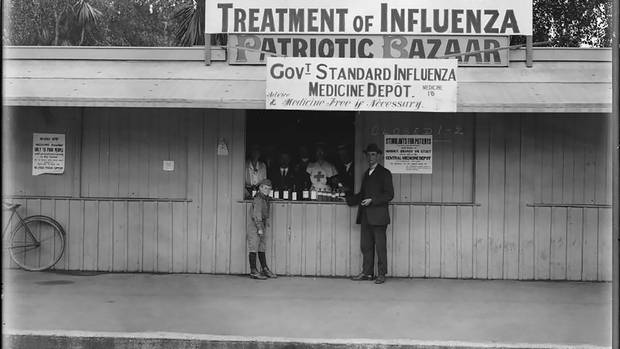
There was no pandemic plan then. New Zealand had early warnings of the infection from events overseas but they were largely ignored, and the government of the day was slow to react. Unlike in Australia, where they enforced strict maritime quarantine, New Zealand didn't close its borders or quarantine troops.
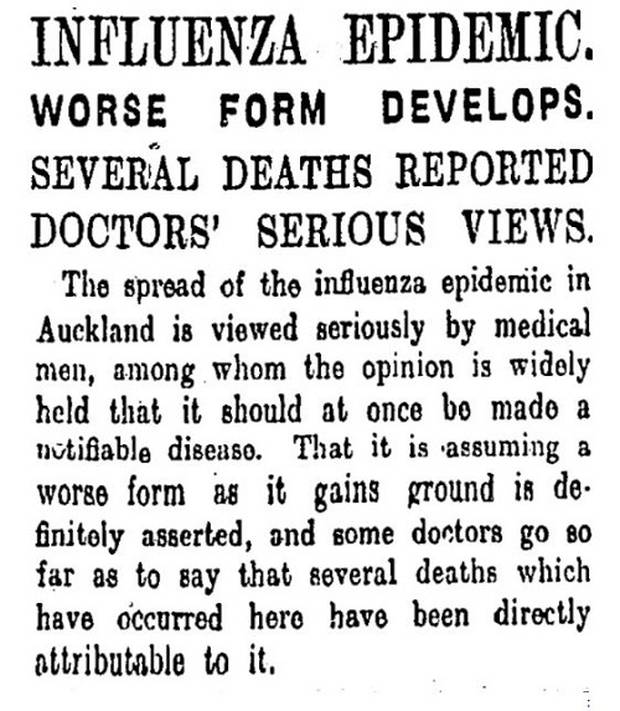
Additionally, people in key positions came down with the flu themselves. In Wellington - where there were twice the deaths of Christchurch, the chief health officer came down with it. So the people who should have taken the lead were in bed, and because of that there was about a week's delay in the response and in that time it spread like wildfire.
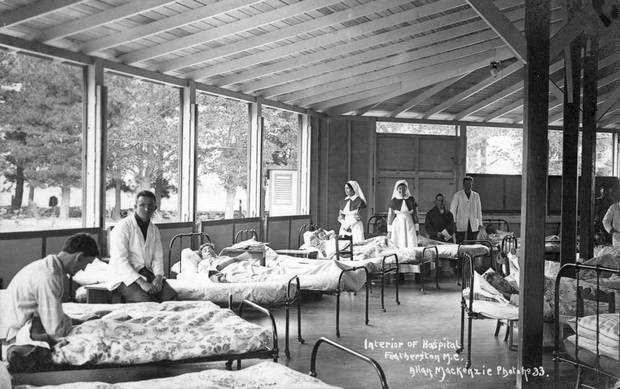
Wellington tried to set up temporary hospitals but by that time many people had pneumonia and were past saving. Christchurch, in contrast, was organised early and well. It has the advantage that it's a more dispersed city, but it also concentrated serious cases at the hospital and kept them there under care of experienced nurses. Whereas in Wellington they had inexperienced people who didn't know how to care for pneumonia - they didn't know about fluid replacement, for example.
Q: Aside from towns like Wellington, who was worst hit?
A: Maori suffered badly, dying at a rate of seven times that of Pakeha. We think that was for a combination of reasons - Maori tended to live in isolated, rural areas, and so weren't exposed to the flu's first, milder wave earlier in the year, and so probably missed out on some immunity. Also they had lost their land and had very poor nutrition and living conditions, tuberculosis was rife, and Maori had high rates of smoking tobacco. All of that likely contributed.
Q: When rules like social isolation were brought in, how did the public react?
A: Remarkably, they kept their heads. But then, they'd had four years of war and people were more accustomed to obeying orders. They helped each other. Whether that will happen now - that's a very good question. I think in 1918 more people were imbued with what they call "Christian values" of charity and helping others in need. I do wonder if we still have that in New Zealand, because after Rogernomics, it's been all about individualisation, greed, all that "me, me, me" attitude. Although the reaction to the Christchurch earthquake cheered me up. The community response is fantastic. But an earthquake is very different to a pandemic and we have no way of predicting how long it's going to go on.
Q: What lessons can we take from all of that as we prepare for Covid-19?
A: The big lessons from 1918 were that delay is dangerous and complacency kills. Acting quickly, as our government has done, is best.
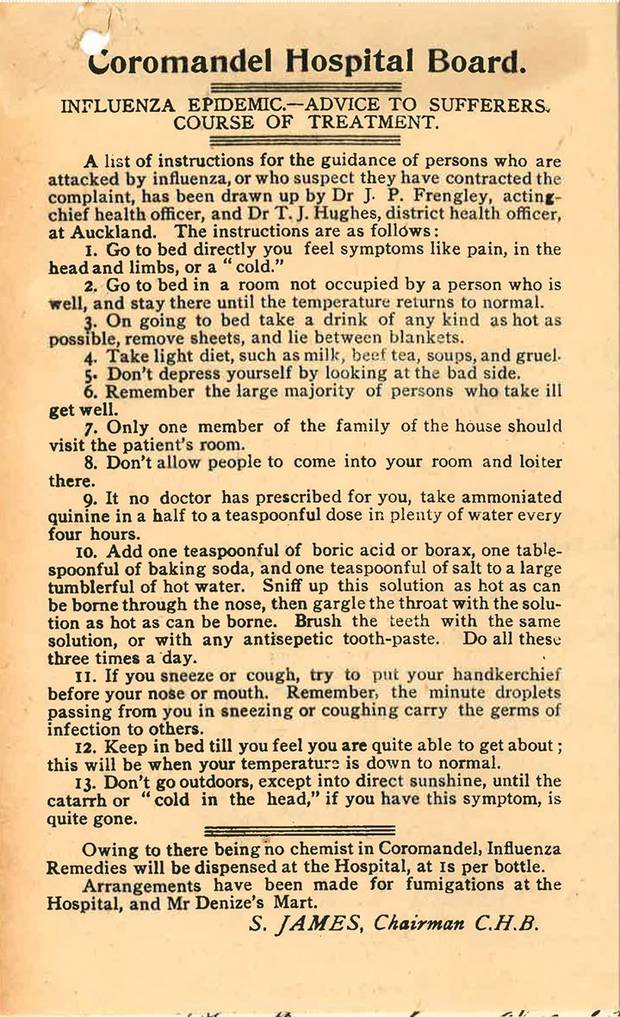
The legacy was that hospitals will inevitably be overwhelmed if we can't keep it out, and stamp it out - that's why we are hearing about flattening the curve. We also learned that people would have to care for others at home - and the Ministry of Health is publishing information about how to do that.
Community response is really important - we should be strengthening community bonds. You should have the numbers of the people around you, particularly if you live alone, or for older people. Things will shut down. People should cancel meetings and gatherings. And follow the advice about isolating and hygiene. If you can, when caring for others, wearing a mask is a good thing to do too.
Q: How are we going so far?
A: New Zealand is doing well. The Pandemic Plan is a good one, it's a whole of government response. So far we have done the right things - although - I think we were a bit slow in closing the border - but other than that top marks. The thing is, it still could be incubating, but it looks like the message about self-isolation after travel is getting through.

Q: What is your parting advice for us?
Listen to proper advice. Don't listen to rumour, don't read conspiracy theories on the internet. Be careful what you repeat. Try to stop the rumour mill just as you stop the spread of infection, and encourage others to listen to the experts too.














