The board yesterday considered initial plans for what it could face next year if, as anticipated, Covid-19 moves from being a pandemic disease to an endemic disease in the community.
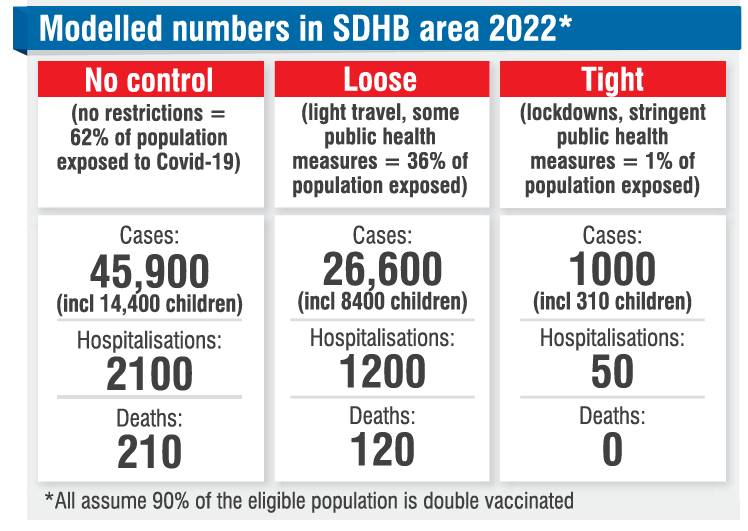
The SDHB’s plans are based on three scenarios provided by the Ministry of Health:
- Unmitigated, where 62% of the population were exposed to Covid-19;
- Loose, where light travel and public health measures were in place and 36% of the population were exposed to Covid-19;
- Tight, where measures like lockdowns were in place and 1% of the population was exposed to Covid-19
Each scenario assumed a vaccination rate of 90%.

‘‘That would relate to 41 hospital admissions a week, 100 emergency department presentations and four deaths.’’
Of those cases, just over 14,000 would probably be children, Dr Lloyd said.
‘‘This is not the number of patients we would expect in our hospitals. You would have to multiply them by length of stay, and the average length of stay of a Covid patient is seven days ... and similarly for intensive care units.’’
‘‘Loose’’ public health controls would likely result in most figures being halved, Dr Lloyd said.
‘‘Cases per week would drop to 24, ED attendances would drop to 60 and the number of people needing ventilation to two, and cases in the community would drop from 880 to 510.’’
‘‘Tight’’ lockdown-type requirements would cause a significant drop in numbers, ‘‘but clearly these measures are completely socially unacceptable’’, he said.
Assuming a lesser measure than tight regulations were in place, it would be crucial that public health tools such as contact tracing were effective, Dr Lloyd said.
‘‘If you don’t have enough resources in that space then the likelihood of that unmitigated scenario happening is much, much higher.
‘‘Clearly for 2022 we have to balance business as usual and dealing with Covid, and we all know that the system is already under considerable pressure.’’
An effective public health system had been the key tool in reducing the impact of the initial wave of the pandemic and it would need to perform excellently once again, Dr Lloyd said.
‘‘The second layer of our response will be primary care and welfare, and finally it is hospital-based systems,’’ Dr Lloyd said.

In an unmitigated scenario, Dunedin Hospital would need to have three wards solely dedicated to Covid-19 cases, and there would be limited capacity for any other patients, he warned.
SDHB chief executive Chris Fleming said the scenarios were worrying.
‘‘When I see these numbers, it is a big number that we have to be prepared for.
‘‘We are going to have to be nimble to react in a timely way.’’
Board chairman Pete Hodgson expected there would be mitigation in place and the worst-case scenario was unlikely.
‘‘We will be needing the active, intelligent support of society to help us through this.’’













