Director-General of Health Ashley Bloomfield has held a briefing about how high vaccination rates affect the response to Covid-19 including hospitalisation rates.
Dr Bloomfield was joined by Immunisation Advisory Centre director Professor Nikki Turner and Tamati Shepherd-Wipiiti, who is the general manager equity for the Covid-19 Vaccine Immunisation Programme.
Dr Bloomfield says this time last year, people were desperate to put a figure around what vaccination coverage could be achieved, and the figure being bandied about then was about 70 percent.
"We know because of Delta that we need to get higher coverage than that."
The 90 percent vaccination milestone is higher than what we would have initially imagined but we need to keep going, he says, it is not a target - it is a milestone.
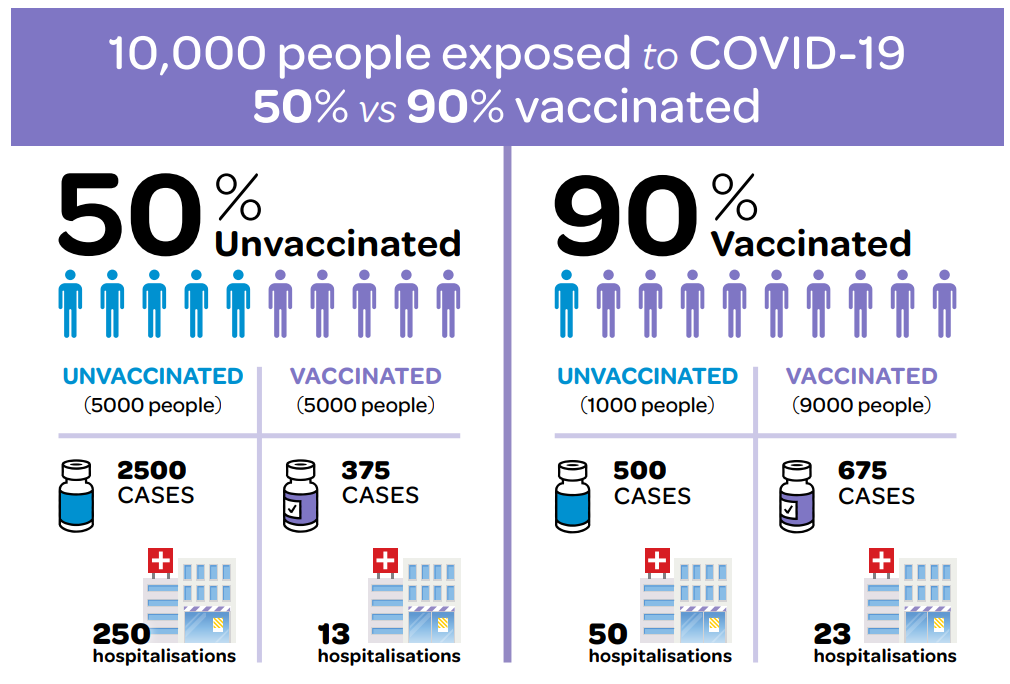
As we get higher vaccination coverage, a larger proportion of people going into hospital will have been vaccinated, but there is an explanation for that, Bloomfield says.
"We're often asked, why 90 percent." Bloomfield says modelling shows 90 percent coverage gives a very high level of protection to the population and it is imperative to be able to manage the response to the ongoing Delta outbreak.
She says it is really important to have high coverage throughout all the communities.
"As Ashley has mentioned, 90 percent is not a magic bullet, we're not going to get rid of Covid with 90 percent coverage, so what we're looking at going forward is obtaining as high coverage as possible. The higher we get, the less hospitalisation we'll see, the less death we'll see.
"We could get really high coverage over there, but If we've left this community behind, when Covid arrives it will find that community.
"There is no point having a highly vaccinated central Wellington when small rural towns are missing out. Covid will find them."
Bloomfield says there is really good data from the Auckland outbreak that shows the virus has not been spreading in settings like supermarkets, and the traffic light system will reduce unvaccinated people mixing with vaccinated people in the settings where it does spread.
A recent Swedish study of more than 800,000 families shows if one member of the household was immune - already vaccinated or recovered from the virus - that reduced the spread to the household by about 45 to 61 percent. With two people immune, it increased to about 75-86, with three immune it rose to over 90 percent, and with four people, the spread reduced by over 97 percent.
That was not a study with Delta, but a recent Dutch study that does include Delta shows a vaccinated person who catches Covid-19 has a roughly 63 percent lower likelihood of transmitting the disease to the household.
Prof Turner says GPs can instantly see who has and has not been vaccinated, and will either phone them to encourage them to get vaccinated or refer them to others if the person cannot be found.
She says the ministry has reached out to GPs to offer extra support with this too.
Children
Bloomfield says 90 percent of 12+ age groups equates to about 76 percent of the total population, and the opportunity to vaccinate under-12s would be a really good opportunity to increase our protection.
He says there is randomised, controlled trial evidence now - "relatively small study, 2000 to 3000 kids" - but New Zealand will be able to look at safety profile as the vaccine gets used for younger age groups in the US.
Prof Turner says the early clinical data looks very good, but the early American data also looks very good.
Shepherd-Wipiiti says some Māori and Pacific communities feel guilty, which is one of the things that might be causing them to be hesitant (i.e. 'I don't want to come in if I can't vaccinate my kids').
He says the Swedish study shows that actually you can take the first step to protect your kids, and clearly shows the more people are vaccinated the more you can protect your kids.
"This rips the heart out of our communities, [that] our kids are getting Covid."
Reducing risk of death and severe illness
The UK office for national statistics has just released data showing the age-adjusted risk of death is 32 times higher for unvaccinated people compared to vaccinated, Bloomfield says.
"That is profound difference. There are very few things I can think of in my public health and medical career that have been so protective and reduced the risk of death so much with such a simple and cheap intervention."
All those who have come out and been vaccinated are doing themselves a huge favour, he says.
However, the increase in the proportion of vaccinated people creates a "sort of counterintuitive thing" where more vaccinated people become cases.
Bloomfield says it was not long ago there was a roughly equal split between vaccinated and unvaccinated.
At that time, based on the protective effect of the vaccine, with 10,000 people, about half of the unvaccinated people would become symptomatic cases, leading to 250 hopitalisations. On the other hand, over 90 percent of vaccinated people do not become symptomatic.
"Even if ... the virus does come in contact with them, their body is able to get rid of it before they become infected or infectious to others."
With 90 percent of a 10,000 population fully vaccinated, it means 500 cases and 50 hospitalisations among the unvaccinated. There are a larger number of cases among the vaccinated population - "it's just simple maths, but even then less than half the number of hospitalisations amongst those cases".
He says the key thing is vaccination greatly reduces the likelihood someone will become a symptomatic case, and greatly reduces the likelihood of hospitalisation or death.
Prof Nikki Turner says the Pfizer vaccine is one of the best in the world - if not the best - performing, and we now have extensive data from around the world. The side effect profile has been clearly delineated.
About one in 12 unvaccinated people who got Covid-19 in New Zealand end up needing to go to hospital*. Dr Turner said about 1 to 2 percent of unvaccinated people would die, and "from the more recent data over 50 percent still have symptoms up to six months later".
She says with concerns about myocarditis - which can be a side-effect of the vaccine - the risk of getting that from the disease is about four times higher than the (very low) risk of getting it from a vaccine.
Equity in vaccinations
Tamati Shepherd-Wipiiti says he wants to celebrate some of the firsts for vulnerable communities including overseas in America and Canada.
He says disability communities are doing really well, and there was a 3 percent to 4 percent uplift in vaccination rates on Super Saturday.
Pacific organisations are smashing their targets, supported by churches and DHBs.
But he wants to celebrate some of the firsts for Māori. The first vaccination in New Zealand was a hauora in Auckland, the first mobile vaccination service in New Zealand as a hauora, and the first kaimahi to be trained to work alongside nurses was a hauora in Tairāwhiti.
In Northland, DHB clinics are getting in about 48 percent of the population, hauora are covering 25-28 percent, and GPs and pharmacies about 22 percent, he says.
What that means for Māori is 77 percent first dose and 61 percent second dose, he says.
There is a large number of rangatahi who need to get vaccinated and there has been a massive uplift in rangatahi coming out to get vaccinated, he says.
Before Super Saturday, Māori vaccinations averaged about 2000 to 3000, and that has since increased to about 5000 a day.
He says the key question is whether there will be another vaxathon, but "the second movie's never as good as the first", so it seems unlikely.
Shepherd-Wipiiti will be hosting a "fried bread friday" in Kaiti, in Gisborne so people can get vaccinated and get a fried bread.
"It's trusted relationship, right."
Māori and Pacific providers like Te Puea Winiata and Silau at South Seas are working closely together to address the vaccine challenge and prioritising things like manaakitanga, he says.
A number of Pākehā are also preferring the Māori health providers, he says.
"We can see a lot of Pacific and I think Māori health providers really coming to the fore, to the front of healthcare service delivery. It's a really beautiful thing to see."
He says iwi have been doing detailed planning about vaccination, testing and how to respond if the virus spreads into their communities.
Bloomfield says there have been really high testing rates amongst Māori, the highest rates of anyone recently, partly because that is where the majority of the latest cases have been.
He says modelling so far shows up to 200 cases a day on average by the end of the month, and there may well be several thousand Māori who have been infected by the end of the outbreak.
Shepherd-Wipiiti says the other flip being seen is a lot more door-to-door initiatives, and the first question was 'how are you whānau'.
"Really important that they were using data that could show them down to which streets.
"We've worked in partnership with iwi, in particular through our data sovereignty group ... to help our iwi access their own data. They've got the toolset ready, if the iwi need a user ID they're ready to go.
"In the Māori world that's not just data, that's our whānau."
Bloomfield says the data will be shared with the Whānau Ora Commissioning Agency. He has signed off the sharing of data for rohe including Tāmaki Makaurau and Kirikiriroa, as well as sharing it with the agency's providers on the ground and with iwi in Waikato.
"It will be shared where those appropriate conversations have happened."
* Prof Turner incorrectly stated on the live broadcast that one in five people who caught Covid-19 would need to go to hospital and need support to breathe. This incorrect figure was based on a misquoted statistic and Prof Turner has retracted the statement.












