Rural people have a higher mortality rate than city-dwellers and the New Zealand health system should redefine what "rural" means to ensure people who live in those areas have fair access to healthcare, new research suggests.
An article published in The New Zealand Medical Journal today argues for a review of the current "rural" criteria.
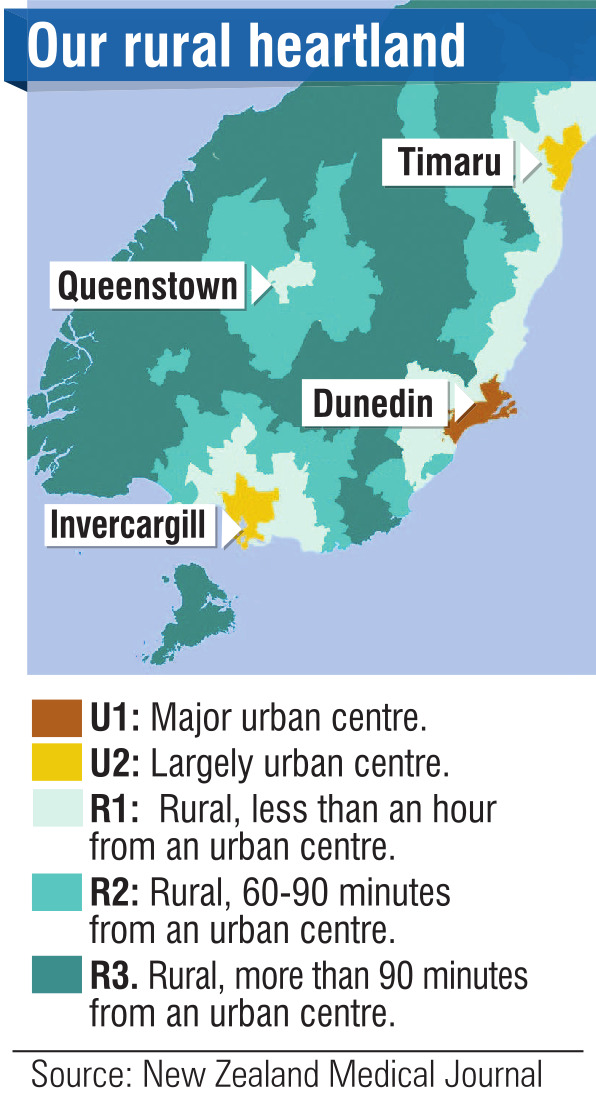
A group of authors, which included University of Otago academics, resurveyed New Zealand on an internationally recognised "geographical classification of health" (GCH) basis and then examined how well the enrolment data of two primary health organisations — one being WellSouth — matched both the old and new maps.
The methodology commonly used in New Zealand had a 70% match to WellSouth’s data, while the new geographic survey was rated almost 95% accurate.
"The GCH is not only a novel and significant contribution to rural health research in New Zealand, but it will help to lay the foundations for improved quality and quantity of rural health research," the article said.
"By demonstrating that rural-urban disparities do in fact exist this work justifies a more thorough examination of the rural context."
Otago associate professor of general practice and rural health Garry Nixon said the GCH results were surprisingly different from either the old or newer Stats NZ classifications of "rural".
There was some early evidence that the GCH-assessed rural population had different health outcomes.
Unadjusted mortality rates in rural areas were as much as 21% higher than in urban areas, a difference which had not shown up when generic statistics were used.
"Inaccurate grouping seems to have been masking real differences in the health outcomes between rural and urban communities," he said.
"Currently, analyses of rural health outcomes often consider those in the commuter zone of cities to be rural, and this means that the relatively good health outcomes of some of the wealthiest communities in the country have been masking the reality of poorer outcomes in many rural and remote areas."
Lumsden Medical Centre owner Mathew Stokes said isolation was the biggest issue which faced rural practices.
"The patients are so far away from facilities and we have to practice according to those needs, for example the results of blood tests are quite often returned about 10 o’clock at night.
"If we are concerned about somebody we either have to forward plan ahead to try and get them admitted earlier, which can put more stress on the local hospital, or we have to wait and then try and arrange something late at night — it’s not uncommon for us to have to get someone out of bed and send them to hospital."
Coupled with isolation, distance — both from rural GPs and from city medical facilities — was an issue, Dr Stokes said.
The stoic nature of rural folk could also be an obstacle to good healthcare.
"Rural people will often put off health needs significantly longer than they should and present quite late and say they couldn’t do anything because they had lambing, or they had calving, or couldn’t get time off.
"That means that they can have worsening conditions which could have been treated more easily if seen sooner."











