By Kate Newton of RNZ
Private hospitals are consistently picking up easier cases from the public system, data shows.
Senior doctors say the numbers are unsurprising, but risk creating a two-tier system, along with burnout in the public system, as staff are left treating the most complex cases back-to-back.
Outsourcing the easier procedures also has implications for training, with junior doctors left with fewer simple cases on which to hone their skills, they added.
However, the Private Surgical Hospitals Association said the data did not back up doctors' concerns, with the numbers showing a small decrease in overall complexity in the public system.
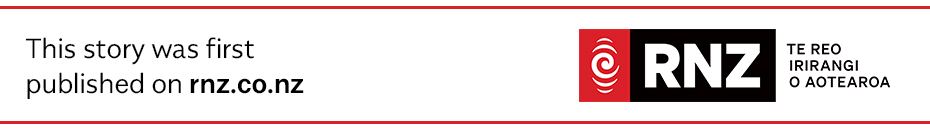
Information released to RNZ under the Official Information Act shows that, since the 2017/18 financial year, the average complexity of elective cases outsourced from the public system to the private sector has been 0.2-0.3 case-weights lower than procedures done in public hospitals.
Case-weights are a way of defining the complexity of surgery.
A case-weight of one would suggest a procedure of standard complexity, with anything over one more complex than normal and anything under one less complex.
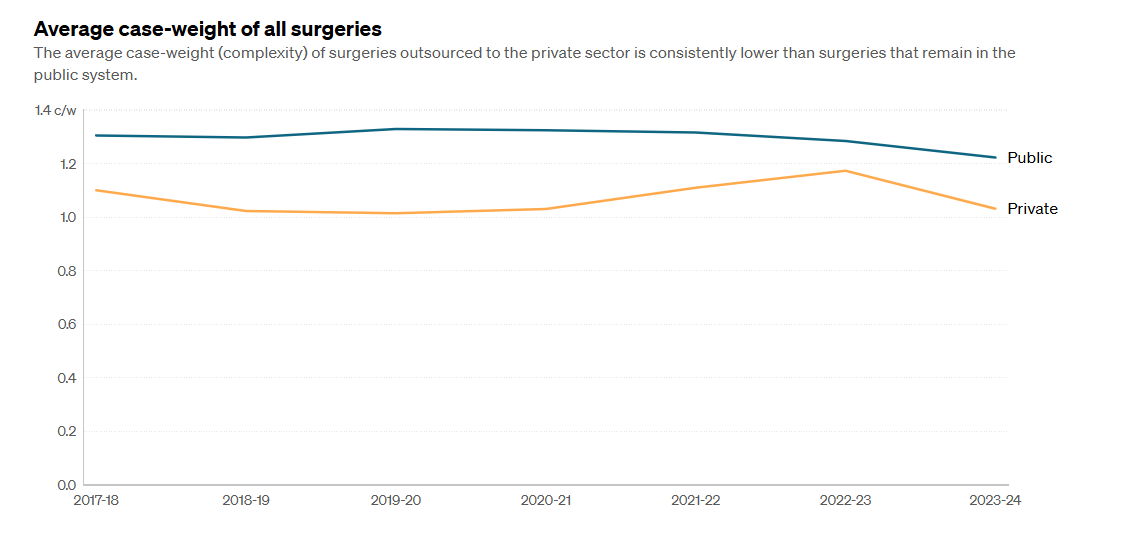
Across various surgical specialties, cases that stayed in the public system were almost always more complex than those outsourced to private.
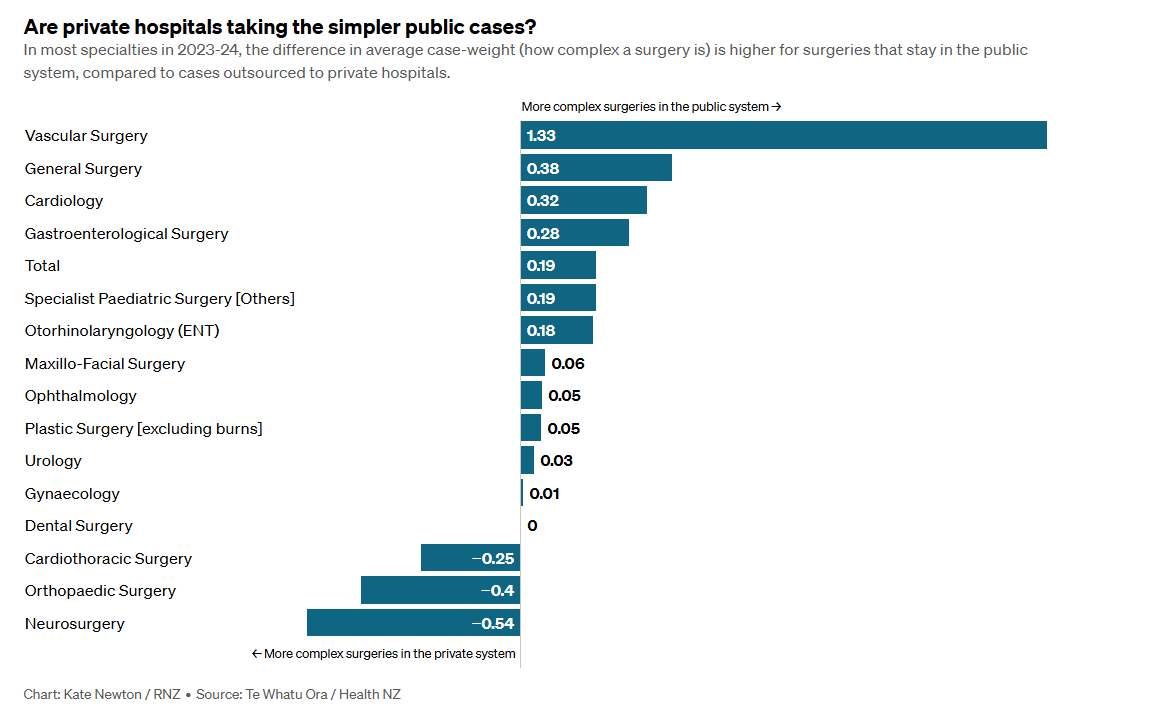
Some of the starkest differences were in vascular surgery - where elective case-weights in the public system were more than double those outsourced - general surgery and cardiology.
Of more than a dozen specialties, only three had higher average case-weights in the private system - neurology, orthopaedics and cardiothoracic surgery.
Neither doctors themselves nor private hospital representatives were surprised by the data, saying private hospitals in New Zealand were generally not set up to handle high-risk patients who required complex pre and post-surgery care.
Private Surgical Hospitals Association chief executive Chris Roberts said only four private hospitals, all of them in main centres, had intensive care units to look after those patients, while another eight had high dependency units.
Three-year outsourcing contracts signed recently between Health New Zealand (HNZ) and private hospitals explicitly guaranteed high-volume, low-complexity patients.
Since 2018, the number of publicly funded procedures completed in the private system has nearly doubled, from 16,000 to 31,000.
Association of Salaried Medical Staff president Katie Ben, whose union represents senior doctors, said although the differences in case-weights were expected, a sustained and deliberate increase in outsourcing had consequences.
It would speed up the wait for low-risk patients with easier procedures, the anaesthetist said, but that would not necessarily translate into faster surgery for complex or high-risk patients remaining in the public system, because the same senior doctor workforce was servicing both sectors.
"You can outsource a whole lot of routine hips and knees to the private sector, which is fine, but if you get a senior orthopaedic surgeon with a particular skillset and management of a particular [complex] case, and they are in private doing their outsourced hips and knees that day, they're not going to be available in public to do that particular case - so it waits until they get back."

Senior doctors have gone on strike this year, most recently in September, over pay and recruitment.
Ben said outsourcing the easier cases had other unintended effects.
"The work at public is going to be harder for everyone - clinicians, nurses and ward staff," she said.
"It means that you're working at the top of your scope all the time - all the time and then some."
ASMS chief executive Sarah Dalton said she worried that was "the route to burnout" for the union's members.
"Also moral injury, because you know that you're not keeping across all the other things as well."
Ben said continued outsourcing would have "a massive impact" on junior doctor training.
"There are lots of cases that the registrars and the ones that are quite advanced in their training would be able to do on their own, except those are the ones that are going to private," she said.
"There's less hands-on time, there's less training opportunity, there's more reliance on the senior medical workforce."

Ben suggested Health NZ should put the money it paid the private system into staffing public theatres over weekends instead, many of which currently stood empty out of regular hours.
"[In Nelson] we've got six theatres in public. One of them works at the weekend on emergency cases - that's five theatres left empty all weekend.
"There's no reason why you can't do an outsourced list of day cases there."
That situation would be similar around the country, Ben said.
Staff capacity, including nursing, would need to be increased, and staff would need to be paid weekend rates, "but not nearly as much as you'd be paying them to work in private... and all that investment goes into public health and stays there".
Private Surgical Hospitals Association chief executive Chris Roberts disagreed that increased outsourcing left only the complex cases for staff in the public system.
The data showed the average complexity of cases in the public system had actually decreased over the years.
"I don't know whether that means that there's a small shift in priority in the public sector towards the less complex cases. It's not a major decline but there is a slight trend downwards."
Ensuring junior doctors could complete their training was a recognised issue, he said.
Because a significant proportion of ACC-funded orthopaedic surgery was done in the private system, there was already an arrangement for registrars and fellows in that specialty to carry out some of their training in private hospitals.
"There are long-standing arrangements, which have become a little more formalised," Roberts said.
"Other specialties, I know, are looking at how it's working for orthopaedics to ensure that, if necessary, they can also have some of their specialty training in the private hospitals."
Health New Zealand chief medical officer Dame Helen Stokes-Lampard said the agency had recently begun training pilots in seven specialties in private settings, including high-volume specialties, like gynaecology, and ear, nose and throat.
"Our trainees will remain employed in Health New Zealand, but they will go out and do some high-volume lists and cases with their consultant to ensure they get enough exposure."

It would be "a complete own goal" if senior doctors simply followed the work to the private sector, she said.
"The proportion of work done in the private sector is still very small as an overall part of the total volume of work that's done in Health New Zealand.
"We're talking about 16,000 in the last quarter done in the private sector on a baseline of over 200,000 procedures in the public sector."
Outsourcing high-volume, low-complexity procedures allowed the public system to handle the remaining cases in a "more creative" way, Dame Helen said.
"It's creating capacity in the public sector to look at the way we organise our theatre lists... so we can look at utilising our operating theatre time as efficiently as possible, so we don't have gaps in theatre lists and so on."
She was in contact with chief medical officers around the country.
"They have their finger on the pulse of what's happening with their workforces locally," she said.
"Where we hear those concerns, we try and address them... because it is in all of our interests for the public sector to be as strong and sustainable as possible."