
My body accuses me. Silently it screams, "What have you done?!".
The shock is understandable. Five days ago I consented to be drugged; sliced open through the buttock; tendons, muscles and ligaments cut; the bone-on-bone ball and socket of my right hip sawn off; metal and plastic replacements lodged and screwed into place; hip briefly dislocated again to test for snugness; then sewn up and wheeled out of theatre to a waiting hospital bed.
So, there is no surprise a few short days later, as I wean myself off multiple brain-fogging painkillers, that the traumatised shell of my being cries, "What the ... ?!".
But I am one of the lucky ones. I have health insurance with surgery cover. I have not spent years becoming increasingly, painfully debilitated, waiting for the severity of my joint disease to reach the threshold that qualifies for hip replacement surgery in a public hospital. I am not stuck on one of those waiting lists that have almost doubled nationally and nearly tripled here in the South. I am already eight weeks down the road to a good recovery because money was spent upfront, rather than relying on a public health system malnourished by successive governments that would rather scrimp on need now then pay through the nose for those same people to become unproductive and dependent as they linger and deteriorate.

Today, it is only three months since I got the results of the MRI showing clearly my right hip needed the years of Ibuprofen that kept me mobile and working, although with increasing difficulty. From that moment, as the orthopaedic surgeon surveyed and explained the images, things moved remarkably quickly. The years of paying weekly, surgery-only, health insurance premiums against "what if" scenarios, suddenly paid dividends. The boss was accommodating, accumulated sick leave plentiful. Four weeks later, wearing only a theatre gown and disposable underwear, I was lying on a table in what seemed like a crowded surgery theatre in Dunedin’s private Mercy Hospital and being told to count down from 10 as the cold whoosh of anaesthetic flooded my veins.
Four weeks for me, but months or even years for many depending on our public health system.

Without health insurance, however, people are dependent on an increasingly burdened and under-resourced public health system. In the five years to the end of October, the number of people on the national waiting list for hip replacements nearly doubled to 2090. The average waiting time also almost doubled to 90 days.
In the South, the picture is grimmer. There are 229 people in the SDHB who qualify but are waiting for a hip replacement, a 122% increase on the same time five years ago. The average length of time they are waiting has skyrocketed from 50 days to 134 days.
And that is just hip operations. In September, the SDHB revealed more than 1000 of its patients have been waiting more than four months for elective surgery of various types. Some could have been waiting for two years or more, the health board said.
New Zealand’s health system explicitly acknowledges that demand outstrips capacity. The solution has been a points-based triage system to ensure the number of people who get on to the waiting list does not exceed the financial and staffing resources allocated for elective surgery. Once again, even measured against this questionable system, the South is slipping behind. In the Auckland DHB, for example, someone requiring orthopaedic (bones and muscles) surgery needs to get over 50 points to qualify for the waiting list. The threshold has been the same in the ADHB for five years. In the SDHB however, the threshold in 2015 was 65 points and is now 70.
The result is the anguished experience of people such as the 62-year-old nurse who contacted The Weekend Mix last week.
Severe arthritis and cysts means she desperately needs hip surgery. The pain and lack of mobility forced her to give up work two years ago, well before she qualified for the waiting list, in August, last year. Despite four month targets for treating waiting list patients, she was told the wait for surgery would be 12 to 18 months.
In the meantime, she is on eight daily medications, including 200mg of Tramadol, 180mg of Codeine, 800mg of Ibuprofen and 4000mg of Panadol.
She and her husband have shifted from Dunedin to a small Southland town to reduce costs. The pain disrupts sleep. The medication causes bowel issues. She is concerned she will lose her licence to practice, making it harder to get work after surgery. The whole situation has pushed her into clinical depression.
"It is plain cruelty to have people in this situation," she says.
My wait, was one month. My pain and loss of dignity, all part of recovery.
I think I was on a high a few hours after surgery. Relieved that it was over and drugged-up enough not to feel much discomfort, I joked with visiting family and ordered lamb shank off the bone from the hospital’s renowned restaurant menu. The next couple of days were spent in a painkiller haze that climaxed with a Tramadol-Hydrocodone concoction - the perfect stupefied state for consuming about 8 hours of American reality TV shows. The days and nights were punctuated by excellent food, repeated blood tests and physiotherapist visits that had me taking steps hours after surgery and mounting steps within 72 hours. Dignity evaporated with the need for an enema and then, when that did the job, help cleaning up.
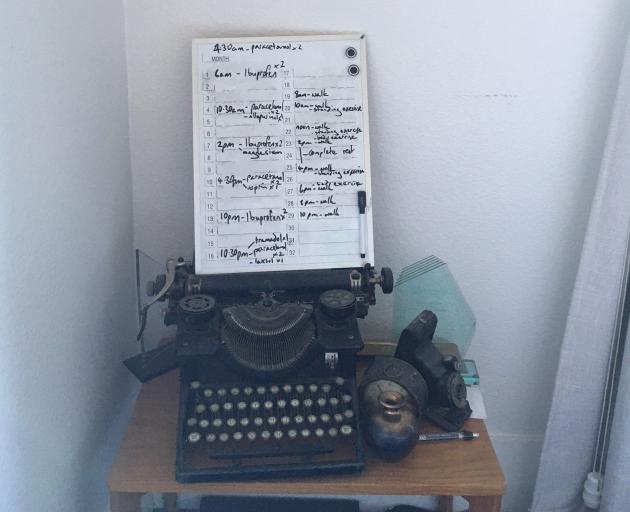
My wife took over nursing duties. She had even typed up a menu and placed a bell by the bed. It took about 24 hours for her to decide caring was not her calling. Trying to keep on top of medications and two-hourly exercise was a losing battle, until we wrote a 24-hour schedule on a small whiteboard and propped it up next to the bed.
The post-op rehabilitation was gaining momentum. For me. Not for all those still on the waiting list, let alone those who have not even made it that far. What is their fate? What should it be?
Researching this article, a request for stories of hip surgery delays was put out on social media. Dozens of people responded online and via email. Including a doctor, who did not want to be named for fear of what it could do to their career.
"Otago and Southland are very under resourced ... Quite frustrating from the medical perspective," wrote the doctor who suggested The Mix speak to Assoc Prof David Gwynne-Jones.
Prof Gwynne-Jones is clinical leader of the Orthopaedic Department, at Dunedin Hospital. He has researched and written on elective surgery waiting lists in New Zealand and particularly the lower South Island.
One key conclusion, published in the New Zealand Medical Journal (NZMJ), 2016, was that hip and knee replacement patients in Otago, in 2014, were more severely disabled than those who got the same operations four to eight years previously.
"Patients currently being returned to GP would have qualified for publicly funded surgery during that [earlier] period," he wrote.
A year later, also in the NZMJ, Prof Gwynne-Jones reiterated the point that telling people they did not qualify for the waiting list did not reduce the need for surgery.
"This delay results in waste, added costs to the patient, healthcare system and society, and may reduce the benefit of surgery.
"There needs to be a significant increase in capacity to meet this demand."
Unfortunately, Prof Gwynne-Jones was unable to comment this week. Despite the surgeon’s extensive experience, an SDHB communications staff member suggested the DHB’s executive director specialist services Patrick Ng "is best placed to answer your questions" and said he could get in touch when he returned from leave next week.

Not only is the waiting list situation bad, "it’s worse than it looks", Mr Bagshaw says.
"Successive governments have underfunded elective healthcare and then tried to make it look better in a number of ways."
Waiting list thresholds disguise the true need for healthcare, he explains.
"The nub of it is that a whole lot of people are being told by their GP that it’s not even worth bothering.
"We know there is an enormous amount of buried need."
Research Mr Bagshaw has been involved in, published in the NZMJ, in 2017, found 9% of the adult population had been told by a health professional they needed intervention and had then been refused treatment. That could mean a potential true waiting list of about 333,000 Kiwis.
Underfunding and hiding the true need is not the moral way ahead. It is not even the cheapest, Mr Bagshaw says.
International research, including a comprehensive European Union study, has proved that restricting access to healthcare is "extreme economic folly".
Early intervention is humane and makes sound economic sense because it gets people back to work more quickly and helps them remain independent for longer.
Properly funding the public health system will save money, Mr Bagshaw concludes.
"If this Government, for which I voted, doesn’t stump up and do something really serious about it, we’re going to slip even further behind.
"If we know investing is going to save you dough, there’s just no sense in not spending it."
Whether the Government will heed that call is unknown. Questions emailed to Minister of Health Andrew Little were responded to by the Government’s holiday-period duty press secretary who explained the Minister was away and the questions had been forwarded to the Ministry of Health. At the time of publication, no response had been received.
It is now eight weeks since my hip replacement, 12 weeks since I was told I needed one. Since leaving hospital, I have made great progress with the Three S’s - showering, sitting and ... toileting. I have received much kind assistance from family and friends. My constant and valuable companions have been crutches, a long-handled grabber and a shoe horn. I’m even back to driving; initiated a week earlier than recommended after my musician wife, who had been gigging the night before, was pulled over by Police on Christmas Day on the road between Omarama and Tekapo for driving too slowly.
The new hip is largely without pain but feels a little clunky. My brain knows there is alien hardware inside.
My right foot wants to point inwards when I walk. There is a lot of supporting muscle to be rebuilt.
But that is all part of post-operative rehabilitation. I can look forward to swimming, cycling, hiking.
Not so for many, many others.
It would be great to think that waiting lists will diminish, that people will get the surgery they need and the health they deserve, that my private health insurance surgery cover will become an uneconomic gamble. But right now, unfortunately, it is gold.
Comments
i just don't understand governments not wanting to fund the health system, yet they have a Minister of Health - why? And i have never understood why Mercy Hospital is soooooo much better than our public health hospital - why? Do our people not deserve equality?
Not 'better'. Collegial. I think public funded procedures are carried out by Marinoto clinicians.
We make noises about being a patient centred healthcare system, but we are not. NZ public healthcare is a deficit driven system designed to minimise intervention in the name of cost savings. Successive health ministers from both National and Labour have done nothing to change this, or change the prevailing attitudes within (Director-General Ashley Bloomfield’s) Ministry of Health. Heaven forbid we have to deal with a true Covid outbreak here. We have one quarter of the ICU bed capacity per capita of Lombardy, and that didn’t go very well did it?
It's shameful the govts have underfunded health so consistently. It's shameful that funds are available for spin-doctors, aka communications, instead. You wrote "an SDHB communications staff member" - an, singular. How many of them are on the payroll?
It's disgraceful that these employees (what's the communications staff budget, can ODT find out?) are used to prevent real workers with long experience of treating as well as being prevented from treating actual pain-wracked patients, from telling the facts.
What, if anything, has gone wrong with investment culture - investment in people not projected profits from yacht races - that makes it reasonable to have e.g. a nurse not only suffering but unable to work in a NECESSARY (or was that only during NZ's Covid lockdown) occupation?
NZ's health system is an embarrassment, especially when we witness innumerable other govts spending follies year after year.
I would have thought the real question that needs to be answered is why it takes Bruce Munro’s experience of the health system to make a small ripple in the media?
This pathetic state of affairs has been the norm for decades and is considered something to be endured by most, except those that have the extra $.
The duplication created by our current DHB model needed a serious overhaul long ago but like our government run education system, it’s captured within political forces that elected officials won’t challenge.
Welcome to the ‘rewards’ of a command driven, as apposed to a market driven system.
Time that the "points" system was overhauled. We are one country. Why should anyone living in the South have to have more "points" than those living in the North? Completely unfair and undemocratic
The question we should be asking is why do we have different points systems for different areas of NZ?
Are we not one country?
Are we not a team of 5 million?
Do we pay less tax than those in the North?
There should be no difference in when people get treated, no matter where we decide to live. We are one country, we have one health system, yet we in the South are discriminated against.












